Age-Related Macular Degeneration (AMD)
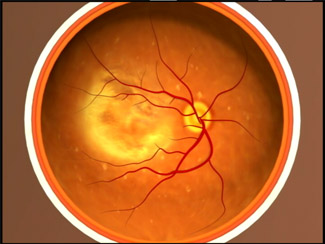
The macula is located in the centre of the retina, the light-sensitive tissue at the back of the eye. The retina converts light into electrical signals and sends these to the brain. It is the macular region of the retina which is responsible for detailed vision and colour perception.
Age-related macular degeneration (AMD) is a disease that blurs the sharp, central vision you need for ‘straight-ahead’ activities such as reading, sewing and driving. It does not affect peripheral vision and does not cause any pain. Of those aged over 60, it is estimated that 25% have some degree of visual loss because of AMD, that equates to more than three million people in the UK. Of these, half a million may have the late stage and this number is thought to be increasing by over forty thousand a year. You can read a report commissioned by the Macular Society into the prevalence of macular disease here.
Risk factors for macular degeneration include:
- Ageing
As we age, cell regeneration declines which increases the risk of developing the condition. - Smoking
Smoking damages blood vessels and the structure of the eye. Smokers are twice as likely to develop macular degeneration than non-smokers. - Family History
There appears to be a ‘Macular Degeneration Gene’ so those with a strong family history are more at risk. - High Blood Pressure
People with raised blood pressure are more likely to have age-related macular degeneration. - Female Gender
More women than men are diagnosed with age-related macular degeneration. - Prolonged Sun Exposure
Macular cells are sensitive to the ultra violet (UV) radiation and visible blue light which occurs naturally in sunlight. Cell damage from blue light may cause deterioration of the macula. - Diet
Diets lacking in antioxidant fruits and vegetables, along with those high in hydrogenated or saturated fats, increase the risk of developing AMD
Smoking and AMD: Studies show that smoking is linked to a two-fold increase in the risk of developing AMD. However, large clinical trials sponsored by the National Cancer Institute showed that beta-carotene (used in AREDS) increases the risk of lung cancer in current smokers (most were heavy smokers). Many studies also suggest that former smokers maintain some increased risk of lung cancer for years after stopping smoking. Therefore, it is reasonable to expect that beta-carotene may also slightly increase their risk of cancer, at least for a period of several years. The risk has been confirmed in the AREDS2 trial. Therefore it is advised that smokers do not take the high doses of beta-carotene in the original AREDS formula. This is one of the reasons for the new AREDS2 formula suggested by the results.
There are two different forms of AMD: wet and dry.
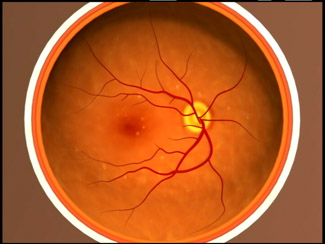
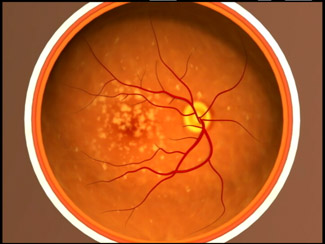
‘Dry AMD’ is the more common form (it should not be confused with having dry eyes) and accounts for about 90% of all cases. It develops gradually over time and usually causes a mild to moderate loss of vision. Drusen, small fatty deposits, are a key sign of AMD and they accumulate at the central part of the retina in the tissues beneath the macula, leading to thinning and drying. The extent of vision loss is related to the location and amount of thinning caused by the drusen. Dry AMD typically has three stages, which may occur in one or both eyes.
Early Dry AMD: people usually have several small drusen or a few medium-sized drusen. At this stage, there are no symptoms and no vision loss.
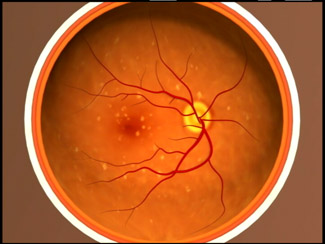
Intermediate Dry AMD: the retina now has many medium-sized drusen or one or more large drusen. Some people see a blurred spot in the centre of their vision and more light may be needed for reading.
Advanced Dry AMD: in addition to drusen there is a breakdown of light-sensitive cells and supporting tissue in the centre of the retina. This breakdown causes a blurred spot in the centre of vision which may enlarge and darken over time. Symptoms include difficulty reading or recognising faces until they are very close to you.
The most common symptoms of dry AMD are slightly blurred vision; difficulty recognising faces; needing more light for reading. Dry AMD generally affects both eyes, but vision can be lost in one eye more quickly while the other eye seems unaffected. Dry AMD may eventually develop into the wet form and cause more serious loss of vision, so regular eye examinations are still important.
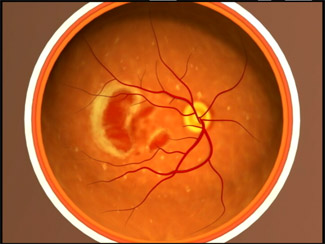
Although ‘Wet AMD’ accounts for only 10% of all AMD, the risk of severe sight loss is much greater. It is caused by the growth of abnormal blood vessels under the macula. These abnormal vessels leak fluid and blood into the tissue at the back of the eye, causing a blister to form in the retina. The resulting scar tissue leads first to distortion and eventually to loss of central vision. Wet AMD can rapidly damage the macula and result in a very quick loss of central vision. An early symptom of wet AMD is that straight lines appear wavy. If you notice this symptom or other changes to your vision, contact your eye care professional for a full eye examination.
The key question is: Are there any treatments for macular degeneration?
Although, there is no proven medical therapy for dry macular degeneration, nutritional supplements have been shown to be of benefit in studies such as AREDS and AREDS2. Have a look at the supplements page for more details.
In recent years there have been several advances in the treatment of wet AMD. Anti-VEGF (Anti-vascular endothelial growth factor) drug therapies have brought hope to many and the list of approaches is growing all the time. Some currently available are Lucentis (ranibizumab), Avastin (bevacizumab) & Elea (aflibercept).
These involve a series of injections into the back of the eye (much less scary than it sounds) which help to inhibit the development of new blood vessels. It is these fragile new vessels that leak and cause the devastating scarring associated with vision loss in wet AMD.
Other exciting possibilities for future treatments include Oraya Therapy (utilising low-voltage x-rays) and gene therapies.
The Macular Society’s website contains a lot of information about various types of macular degeneration, treatments as well as nutritional advice.